The dark side of sun exposure
By Randall Mang
Known as the "dark skin cancer" and the most dangerous form of skin cancer by many Canadians, melanoma is something David Zloty deals with on a far too frequent basis.
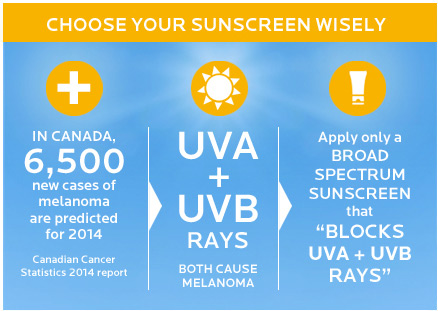
As the director of the Dermatologic Surgery Centre, Dr. Zloty’s schedule is very busy, partly due to an upsurge in skin cancer. For melanoma alone, an estimated number of 6,500 new cases and over 1,000 of deaths are predicted for 2014 in Canada, according to the Canadian Cancer Statistics 2014 report.
Dr. Zloty, who is also the president of the Canadian Dermatology Association, sees prevention as the best course of action. “At the present time, given that we are not able to modify any genetic alterations that increase our risk of melanoma, I feel protection from UV radiation is probably the most important step Canadians can take to reduce their risk,” he says.
As a cancer of the melanocytes, melanoma affects the cells that produce melanin, the pigment that is primarily responsible for giving the skin its colour. When ultraviolet (UV) light strikes the skin, melanocytes make more melanin, leading to a darkening – or tanning – of the skin, as the cells’ attempt to prevent further sun damage. Yet the cumulative effects of exposure to UV radiation cause cell mutations, potentially resulting in abnormal cell function and cancer.
What makes melanoma especially dangerous is its ability to spread through the blood and lymph vessels to other parts of the body. In addition to prevention, early detection is crucial when it comes to skin cancer.
More and more Canadians guard against excessive sun exposure but they need to be better informed, says Dr. Zloty, who recommends year-round sun safety measures, such as wearing hats, clothing and sunglasses, and not scheduling outdoor activities during peak sun hours. “People must also be encouraged to use sunscreen properly,” he adds.
Tanning booths are another concern, says Dr. Zloty, noting there is mounting evidence that using tanning beds, especially before the age of 35, increases the risk of melanoma.
Tanning booths primarily emit UVA radiation. Known as the dominant tanning ray, UVA penetrates the skin more deeply than UVB. The exposure to UVA rays, whether outside or in tanning booths, has long been linked to sun damage.
Even through there is more work to be done in raising awareness about UV radiation, Kateline Turgeon, director of national training for sunscreen and skin care brands La Roche-Posay and Vichy, is grateful for the improvements to date. “In the ‘80s, people were literally lathering their skin with baby oil and used aluminum foil reflectors to increase the number of rays reaching the skin. Fortunately, we don’t see that type of behaviour any more,” she says.
The next step, for Ms. Turgeon, is firmly integrating sun protection into the daily routine of Canadian families. La Roche-Posay recently launched behindthespf.ca, an interactive website that draws attention to UVA and UVB risks.
Since a large percentage of sun exposure happens before we turn 18, Ms. Turgeon believes that education starts with young families, and the message needs to be reinforced in schools. If children grow up regarding sun safety measures as integral part of their outdoor experience, they have a better chance of forming healthy life-long habits.
“Some studies show that using effective sun protection on a regular basis, including adequate application of sunscreen, is helping to reduce the risks of skin cancers, of which melanoma is part of,” says Ms. Turgeon.
When Dr. Zloty speaks to his patients about using sunscreen, he first tells them about preventing premature skin aging.
“Most of my patients want to look their best and dislike the concept of looking older then their age,” he says. “I also speak of preventing sunburns – most patients to not want to shorten holiday enjoyment by missing one or two days of fun because of a painful sunburn. Then I speak of preventing skin cancers, including melanoma, which could potentially harm their health in both the short and long term.”
Once Dr. Zloty has convinced his patients to use sunscreen, he ensures that they choose products that provide UVA and UVB protection. “If the sunscreen package does not say ‘blocks UVA and UVB rays’ or ‘broad spectrum,’ then the sunscreen should not be used,” he says. “I also tell patients to look for the Canadian Dermatology Association logo on a sunscreen bottle that ensures that the sunscreen meets the criteria for effective sun protection.”
Ms. Turgeon says the latest Health Canada sunscreen monograph will soon make it easier for consumers to choose products that offer effective broad-spectrum protection. “A new UVA logo indicates that a sunscreen offers the minimal requirement in terms of UVA protection that Health Canada is looking for,” she notes.
Emphasizing the need for UVA protection year-round and even in the shade, Dr. Zloty says, “It’s been a challenge to impart to our patients that UV radiation can have negative effects on skin health even in winter, on cloudy days, and through haze, fog and certain types of glass,” he says. “To ensure maximum skin health, they should use sunscreen even on cloudy days.”
For his patients with heightened risk factors – such as sun-sensitive skin or a family history of melanoma – Dr. Zloty likes to points out that negative consequences can be severe should they choose to not protect themselves from UV radiation. “In addition, all patients can be provided with written information as to what skin cancers can look like,” he says, adding that high risk patients may require dermatologist assessments on a regular basis.
Read the full report in it’s host publication →
Common misconceptions about melanoma
Although the majority of Canadians are protecting themselves from excessive sun exposure, Dr. Zloty has noticed a few widespread misconceptions about melanoma:
- Melanoma, like other forms of skin cancer, is often mistakenly viewed as "a disease of older people." Yet in British Columbia, for example, it is the third most common cancer in young adults between the ages of 15 and 29.
- "Once you have a melanoma, there is a high chance you will die from the disease," is a widely-accepted assumption when, in fact, the vast majority of melanomas are low risk melanomas, and local excision of the area can prove curative, says Dr. Zloty.
- "All melanomas are brown or black, so I did not worry about this enlarging red bump," is something that Dr. Zloty has heard from patients. While the majority of melanomas are brown or black, he cautions that in some cases, they can be red, or red-blue, or sometimes even skin-coloured. “If something on the skin is changing, it may be best to have a dermatologist assess the area,” he says.
- "The surgery to remove the melanoma will leave me with a very large disfiguring scar," is a concern Dr. Zloty has noticed. Yet he says that with modern excision margins, the vast majority of melanomas can be safely excised and closed, leaving only a long narrow scar with good cosmetic results.
- Some people say they didn't use sunscreen because they’d heard sunscreens do not protect against melanoma. Dr. Zloty, however, explains that more and more studies show a connection between sun exposure, sunbed use and an increased risk of melanoma.